Yeah, robot surgery used to be just a movie thing, you know? Well, it’s here now, and it’s changing how doctors do their jobs.. The ROSA surgical robot is a prime example. It’s known for its ability to really nail the details, move in all sorts of ways, and generally give surgeons a leg up when tackling tricky operations. This thing comes from Zimmer Biomet and is made to help with surgeries, specifically stuff like fixing bones and dealing with brain issues. The whole idea isn’t to kick surgeons to the curb, but to give them a hand, making surgery safer and quicker.
Why Robotic Surgery is Catching On
To get why ROSA is a big deal, let’s talk about why robotic surgery is trending upward. Doctors have understood for years that even surgeons who are at the top of their game can run into problems when things get really complicated. Regular surgery means big cuts, takes longer to heal, and comes with risks. Robotic surgery looks to change this by making operations less invasive, giving the doc more fine-tuned control. These systems show surgeons a better view of what they’re doing, real-time info, and a guided way to position tools. All these things are the reason why hospitals all over are grabbing robots like ROSA to get better results for their patients and shorter recovery times.
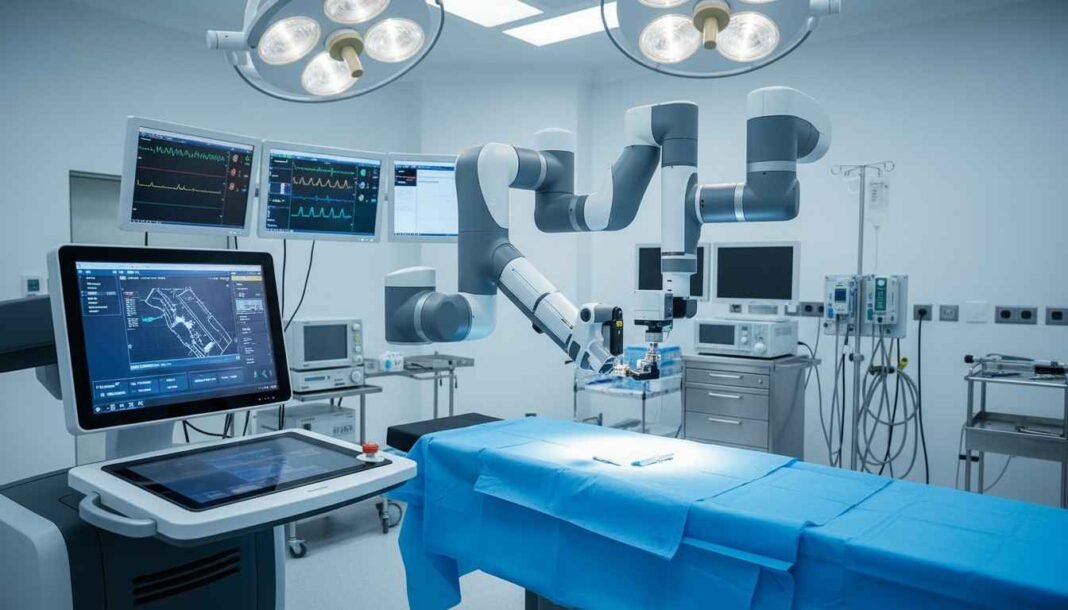
ROSA in Action: How it Works in the OR
Basically, ROSA is like a robot arm that the surgeon controls during the operation. ROSA doesn’t do surgery on its own; every move is based on the surgeon’s hand command. What’s cool is its smart guidance system. Before the knife even comes out, doctors load imaging data, like CT scans or X-rays, into the robot’s computer. This means the robot can map out exactly what the patient’s insides look like. Okay, once the surgeon gets going, ROSA sticks to the plan, so we don’t mess with anything too sensitive. The system is always giving updates, making sure we’re doing exactly what we meant to do from the start.This prevents mistakes and makes the surgery less of a guessing game – as accurate as can be. Everything is meticulously planned out and is just a steady process with great results and no complications.
ROSA's Impact in Neurosurgery
Neurosurgery was one of the first areas to latch onto ROSA. Surgery on the brain and spine has to be spot-on because even a tiny slip can screw things up big time. ROSA helps neurosurgeons during things like deep brain stimulation (DBS), biopsies, and handling epilepsy. If you are having trouble moving because of Parkinson’s, surgeons can use ROSA to put electrodes in your brain safely and get rid of shaking and stiffness. Before ROSA, these surgeries took longer and were riskier. Now, with the robot, placements are more exact, so healing’s quicker, and you often have fewer problems later.
ROSA's Growing Role in Orthopedic Surgery
Another big area where ROSA is starting to shine is fixing bones, especially knee replacements. You’ve got to get the knee lined up just right in a replacement, or it’ll mess with how you move and feel. ROSA gives surgeons a hand by measuring the bone structure and guiding how implants are placed to match the patient’s natural movement. During the op, ROSA is always collecting up-to-the-minute info from the area and can help tweak the plan if needed. In the long run, You will be feeling better for years to come due to how accurate the procedures are and how they take live data, making a better outcome. It feels more natural, and you will be happy you are walking around after the recovery period. Doctors find that patients getting ROSA-assisted knee surgeries have a smoother time with pain, rehab faster, and feel happier about it all.
The Upsides for Everyone Involved
The good news about ROSA is that it helps everyone. Surgeons get a system that backs up their calls, gives them hard data, and keeps their instruments steady. Instead of just going by feel, they have a tool that helps them be more confident and eliminates some guesswork. Smaller cuts, less infection risk, faster recovery for patients. The precision offered by ROSA lowers the chance of needing a redo later, which is a huge plus. A lot of times, patients say they feel better and more comfortable after ROSA-assisted procedures.
The Not-So-Good Stuff
For all that’s good, there are challenges. The big one is cost. These robotic systems cost a ton to buy and keep running, which can drive up the price of surgery, especially for hospitals that are already strapped for cash. Surgeons also need to train a lot to use ROSA right. If you don’t know what you’re doing, the robot can’t do its thing. Also, some people worry that tech may take away from the real experience of the surgery, But for good measure, most surgeons would say that it helps them. Technology always gets better, and people are always pushing to improve ROSA to make it more affordable and available.
Stories from the Field: ROSA in Real Life
Loads of hospitals are telling success stories with ROSA. Brain surgery patients are seeing better outcomes; less time in operations. Knee replacement folks are comfortable and steady on their feet. Surgeons rave about how the system helps them stay precise during long, tough ops. These are actual results. These real outcomes stress the real-world benefits of robot help. In the world of medicine, numbers are the most important, and both in trials and in the daily lives of hospitals, ROSA has shown great numbers repeatedly.
Looking Forward
The ROSA surgical robot is just one part of what’s changing healthcare. As more hospitals pick up robot systems, surgeries are likely to get safer, quicker, and better fitted to the individual. Developers are still working to give ROSA better software, more movement, and help with more kinds of surgery. Eventually, the robot may be helping out in areas beyond the brain and bones. Surgeons are necessary and won’t be replaced but robots like ROSA will just become more run-of-the-mill but also a tool that can deliver better care.